Hungarian researchers at the Szeged Biological Research Center (BRC) belonging to the Eötvös Loránd Research Network and the Department of Dermatology and Allergology of the University of Szeged studied tumor patients treated with immunotherapy with the aim of identifying the factors that determine the individual immune response to therapy. The study presenting their findings was published in the prestigious journal Nature Cancer on July 8.
The human immune system plays a fundamental role in killing pathogens and tumors, while it is essential to tolerate healthy cells of the human body. Tumor immunotherapy has revolutionized cancer treatment in the previous two decades. The treatment is effective against advanced cancers and has given hope for patients in late stages of the disease. The importance of immunotherapy is well illustrated by the fact that in 2018, researchers who played a significant role in its development, James P. Allison and Tasuku Honjo, were awarded the Nobel Prize in Medicine.
Tumor immunotherapy augments the immune recognition of cancer cells, which could destroy even metastatic tumors. While it was a huge step forward in the treatment of cancer patients, a notable fraction of them do not respond to the therapy. Consequently, it is of utmost importance to identify biomarkers that can predict which patients benefit from the treatment.
HLA molecules make it possible for the immune system to recognize the molecules of pathogens, tumors and healthy cells. They present short protein fragments on the surface of cells and show extreme diversity, resulting in large differences between individuals. HLA variants called ‘generalists’ can bind and present a very large number of protein fragments to the immune system. These variants are more prevalent in geographical regions with high pathogen diversity because they make it possible for the immune system to recognize more pathogens. One would think that generalists are beneficial in terms of tumor recognition because they are more likely to bind and present the mutated protein fragments of cancer cells. Surprisingly, researchers found the opposite.
The team of researchers – led by Csaba Pál and Máté Manczinger – focused on patients treated with immune checkpoint blockade immunotherapy. They showed that although generalists are more likely to present mutated cancer peptides to the immune system, patients carrying generalist HLA variants actually have a worse survival rate. What could be the explanation for this phenomenon?
Unfortunately, generalists are not selective. They also bind and present the original peptides from which mutated peptides arise. As mutated and original peptides are often highly similar, the immune system is unable to distinguish between them and as a result it recognizes tumor cells as healthy ones. On the contrary, selective HLA variants are more likely to present only the mutated peptides, and thus the immune system can recognize and destroy tumor cells more effectively.
The question arises whether carrying generalist HLA molecules is also associated with inadequate immune recognition of pathogens. In their previous research, the team showed that generalists make it possible for the immune system to recognize and destroy more pathogens. This is explained by the low similarity between human and pathogen-associated proteins. As a result, even though generalists do present more self-proteins, the immune system can easily distinguish pathogens from human cells.
In summary, in the case of generalist HLA molecules, quantity predominates peptide presentation at the expense of quality, which results in the defective immune recognition of tumors. The results could help to decide which patients should be treated with immune checkpoint blockade immunotherapy. Importantly, adequate immune recognition of cancer is essential throughout life, which is exemplified by the increased susceptibility of immunocompromised individuals to cancer. BRC researchers are planning to investigate whether individuals carrying generalist HLA molecules are generally predisposed to different tumors as their immune system is unable to recognize cancer cells effectively.
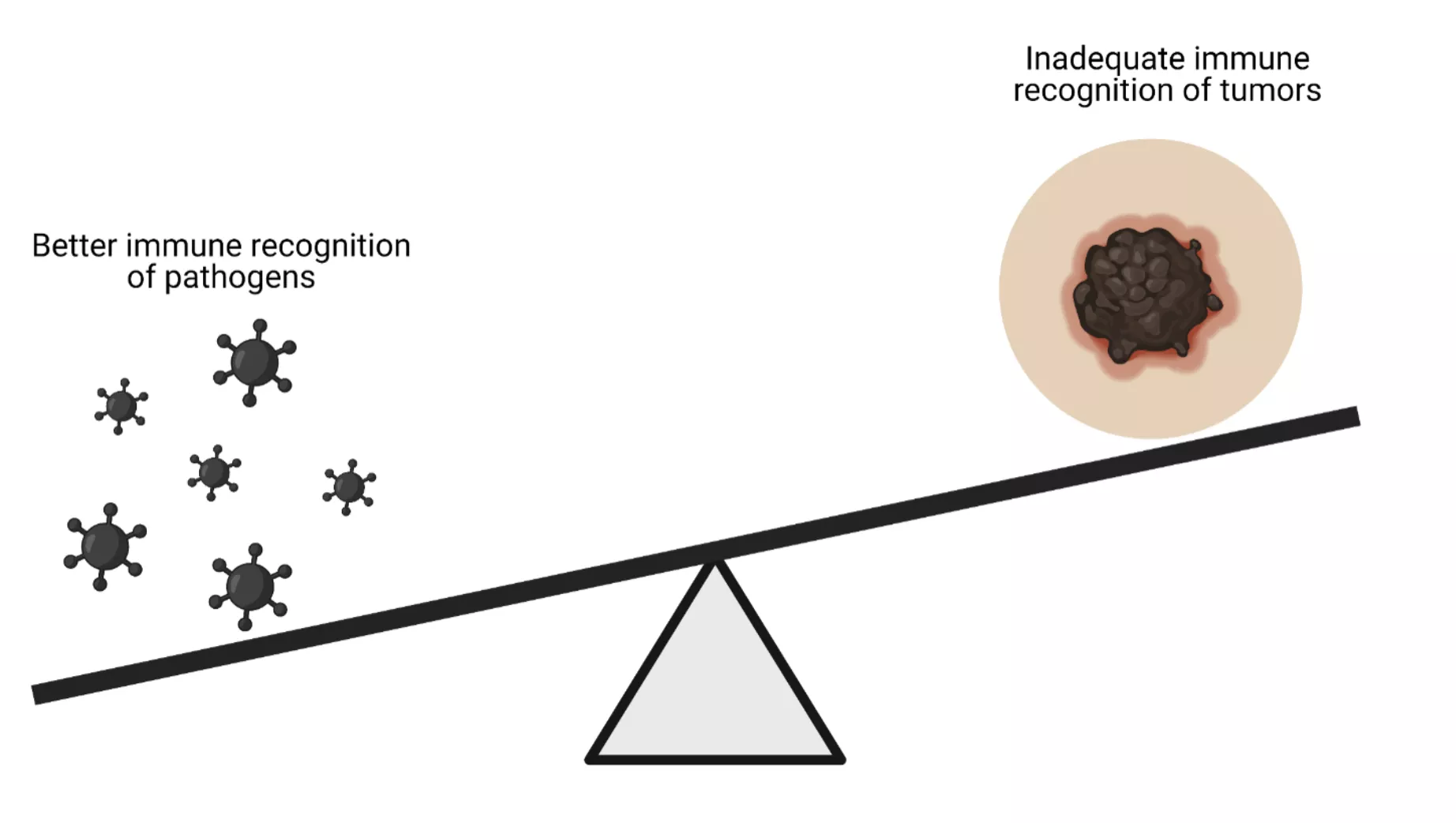
The effect of generalist HLA molecules on the immune recognition of pathogens and tumors. Generalists make it possible for the immune system to recognize and destroy a higher number of pathogens. However, there is a negative trade-off between the recognition of pathogens and tumors. (biorender.com)
Contact:
Csaba Pál (http://sysbiol.brc.hu/pal-csaba-lab-member.html#csaba-pal)
Máté Manczinger (http://immunoinfo.tk, manczinger.mate@brc.hu)